- Summary
Brucellosis, also known as Mediterranean fever or Maltese fever, is a highly contagious zoonotic disease caused by bacteria of the genus Brucella. Human infections typically occur from consumption of infected meat or unpasteurized dairy products. Symptoms of Brucellosis may last for prolonged periods of time and include; fever, fatigue, muscle pain, headache and anorexia. Long term or reoccurring symptoms such as undulating fever, arthritis, endocarditis, neurologic abnormalities, chronic fatigue, depression, hepatomegaly, and splenomegaly, may impact an infected human throughout their lifetime. Treatment for Brucellosis involves alleviating the symptoms of the disease, preventing the onset of new disease, and avoiding long term complications. No cure for Brucellosis is available. Livestock animals with Brucellosis generally experience poor milk production, spontaneous abortion, infertility, lameness and severe weight loss. Vaccination programs, pasteurization of milk, good hygiene practices, and early reporting systems have significantly decreased the incidence of the disease in developed countries. Brucellosis remains a high risk in South America, Eastern Europe, Africa, and the Middle East.
- Facts
| Formal binomial name of microbe: | Brucella suis, Brucella melitensis, Brucella abortus, and Brucella canis |
| Gram stain (gram positive, gram negative or neither): | Gram Negative |
| Is the microbe mobile or immobile? | Immobile |
| Primary habitat? (Where is the organism normally found or prefer to live?) | Tissue of infected organisms (spleen, liver, reproductive organs, mammary glands) |
| Can the organism infect humans? | Yes |
| Can the organism infect other species? If so, which ones. | Swine, cattle, goats, sheep, bison, and dogs |
| Documented cases of antimicrobial resistance? | Yes |
| Number of infections per year in the US | 80-120 |
| Number of infections per year in the world | >500,000 |
- Description
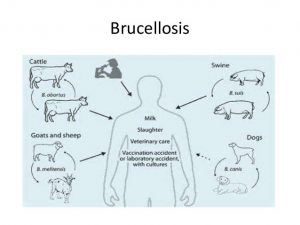
Brucellosis is a highly contagious infectious disease caused by bacteria of the Brucella genus. While many species of Brucella exist, four specific species are typically linked to human disease: Brucella suis from swine, Brucella melitensis from goats and sheep, Brucella abortus from cows and bison, and Brucella canisfrom dogs. In livestock, Brucella species are shed in the milk, secretions expressed during parturition, the tissues of an aborted fetus, or in other reproductive secretions. Contact with these bacteria through ingestion of infected milk or meat, inhalation, contact with mucous membranes or skin wounds leads to Brucella infection in animals and humans. Farmers, veterinarians, slaughterhouse workers, and meat-packing plant employees are at the highest risk for infection.

Brucellosis outbreaks in livestock are detrimental to the livestock industry with the disease decreasing fertility, milk production, overall health and limiting growth of livestock. Methods to eradicate Brucellosis involve vaccination, testing of livestock, herd surveillance, and depopulation of severely infected herds. Brucellosis vaccinations are available but are only 70-80 percent effective in preventing the disease. Brucellosis control methods have decreased the economic impact of the disease on the livestock industry from $400 million annually in 1952 to less than $1 million annually in recent years.
While Brucellosis infection in animals is expensive and detrimental, the transmission of the bacteria and subsequent disease in humans is more concerning. Humans often encounter Brucella species in unpasteurized milk or under-cooked meat. Additionally, humans may become infected with the bacteria from contact with livestock or infected wild animals, occupational infection from laboratory samples, mother to fetus, or blood transfusions. Human to human transmission of the disease is very rare. Once a human is infected by the bacteria, immune cells engulf the organisms and transport the bacteria to lymphoid tissue, specifically the liver and spleen. The lipopolysaccharides in the Brucella species’ cell wall allow the organism to resist destruction by the body’s immune system. The bacteria are able to escape and form colonies throughout the body. The bacterial growth causes symptoms of infection, such as, fever and flu-like symptoms. Generally, the onset of symptoms in humans occurs within five days to five months of exposure.
Diagnosis of Brucellosis infection is challenging for physicians since the bacteria are only found in whole blood samples during the early stages of the illness. Additionally, culturing Brucella species in the laboratory is difficult because the bacteria grow very slowly and require special protective measures to ensure the health of laboratory workers. Physicians often rely on agglutination tests or enzyme-linked immunosorbent assays (ELISA) which utilize serum from a patient’s blood to detect antibodies for Brucellosis produced by the patient’s immune system. Treating Brucellosis infection involves a combination of antibiotics, taken over an extended time period to limit the symptoms of the disease and decrease the chances of long term complications. Physicians utilize a combination of doxycycline or ciprofloxacinare in combination with rifampin but other antibiotics may be used if necessary. Brucellosis is not a curable disease but the symptoms and long-term complications can be managed with antibiotic treatment.
The incidence of Brucellosis in humans is rare in the United States. Approximately 80-120 cases are reported to the Centers for Disease Control annually. Developing countries, specifically regions of Eastern Europe, Africa, South America, and the Middle East, have an increased incidence of Brucellosis in animal and human populations. The World Health Organization estimates over 500,000 cases of Brucellosis are discovered worldwide annually. Individuals traveling to endemic areas should use caution when consuming dairy products or when coming in contact with livestock.
- News Articles
World’s most rapid Brucellosis test designed in Iran
https://www.tehrantimes.com/news/436963/World-s-most-rapid-Brucellosis-test-designed-in-Iran
An Iranian company has designed a Brucellosis test that detects the disease after twenty minutes. Previous Brucellosis testing detection required a minimum of forty-eight hours for a confirmation of the disease. Rapid detection is an important step in controlling this devastating disease.
Researcher Calls for Enforceable Guidelines to Slow the Re-emergence of Canine Brucellosis, a Bacterial Disease That Can be Transmitted From Dogs to Humans
A study by scientists at the University of Iowa calls for more oversight of dog breeders, movement of dogs across state and national borders and increased regulations to limit the spread of canine Brucellosis. Brucellosis infections in dogs are increasing and pose an increased risk to humans as regulations on dog breeders and transportation of dogs are largely unenforceable. Scientists recommend testing of dogs before travel to limit spread of the disease.
School of Veterinary Medicine assists Wisconsin animal shelters with canine brucellosis response
Two dogs transported to a Wisconsin animal shelter from South Korea were found to be infected with Canine Brucellosis during routine diagnostic testing. The dogs were quarantined at the shelter until they were determined to be safe to human and animal health. The University of Wisconsin advised multiple area shelters on appropriate quarantine procedures to ensure that no dogs from area shelters would risk spread of the disease.
- Reference List – Includes a minimum of 3 references. Formatting should be:
- “National Organization for Rare Disorders Rare Disease Database”; https://rarediseases.org/rare-diseases/brucellosis/
- “NCBI Database Bookshelf Brucellosis”; https://www.ncbi.nlm.nih.gov/books/NBK441831/
- “Centers for Disease Control and Prevention Brucellosis”; https://www.cdc.gov/brucellosis/index.html
- “The Center for Food Security and Public Health at Iowa State University Fact Sheet:Brucellosis”; http://www.cfsph.iastate.edu/FastFacts/pdfs/brucellosis_F.pdf
- “USDA APHIS Facts About Brucellosis”; https://www.aphis.usda.gov/animal_health/animal_diseases/brucellosis/downloads/bruc-facts.pdf
- “Brucella- Virulence Factors, Pathogenesis and Treatment.”; https://www.ncbi.nlm.nih.gov/pubmed/30015453
Created by: walack@lcc.edu