Narcolepsy
By: MicKayla Blodgett
Summary:
Narcolepsy is a chronic sleep disorder that causes sudden bouts of sleep and extreme daytime sleepiness. These sleep attacks can last anywhere from 30 seconds to 2 minutes and cause extreme difficulties for those afflicted. People with this disorder can fall asleep anywhere doing almost anything. Where it does have hereditary components, the chance of a parent passing it down to their child is about 1%. Narcolepsy is typically diagnosed between the ages of 10 to 40. In the past it was thought that both men and women are equally likely to have narcolepsy, however recent studies suggest that it may be slightly more prominent in those assigned males at birth.
Description:
Narcolepsy afflicts 3 out of every 10,000 people, although most cases are misdiagnosed or unreported. Narcolepsy is often mistaken for depression, anxiety, insomnia, sleep apnea, ADHD, epilepsy, and chronic fatigue symptom. However, many of these disorders may coexist as a secondary complication to narcolepsy. For example, 57% of people who have narcolepsy also deal with depression, and 53% deal with anxiety-related disorders. Most times, treatment of narcolepsy can drastically improve the symptoms of anxiety and depression these people feel. Narcolepsy can also cause issues with obesity, eating disorders, high blood pressure, high cholesterol, and heart desiese. In fact, those with narcolepsy are 20% more likely to struggle with obesity than those without. This may be due to a slowing of metabolism or not getting enough time to exercise. Narcolepsy also puts those afflicted at a predisposition for diabetes, sleep apnea, arthritis, and chronic pain. These are thought to be linked to sleep quality which explains why those who have a complicated relationship with sleep would experience them more often.
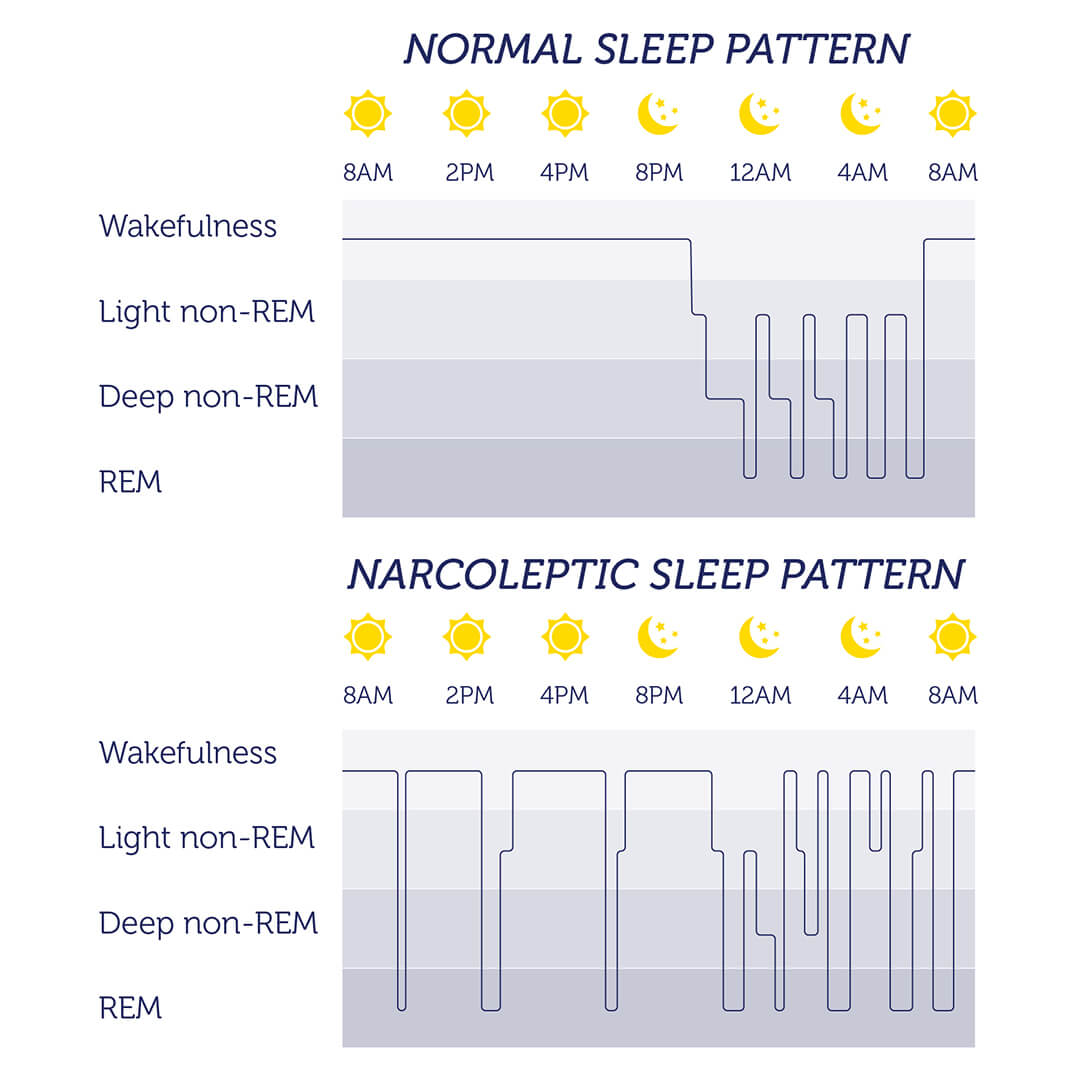
Problems with narcolepsy center around the inability to keep the energy at a consistent level. This can be caused by several things. In the case of type one narcolepsy, a lack of the chemical hypocretin, or cataplexy, which regulates the rapid eye movement (REM), or dream cycle, causes a sudden lack of muscle tone that is triggered by a strong emotion. This may cause slurred speech or the inability to control most muscles. In both type 1 and type 2, patients run the risk of falling asleep while preforming repetitive tasks they regularly perform. This can cause issues with the ability to keep a job, raise a family, and even drive. Because this disorder can cause so much damage to a person’s life, there are several ways to treat it.

Although narcolepsy has no cure, scientists are consistently finding new ways to help those afflicted. Scientists have found that taking brief naps throughout the day and setting a strict bedtime help the body better regulate the REM cycle. Also, patients are encouraged to watch their intake of sugar, carbs, spice, alcohol, and caffeine as any one of these factors can decrease nighttime sleep and increase the effects of narcolepsy. In some cases, CBD oil increases wakefulness in those afflicted. If symptoms continue to progress after a patient has tried all of these methods, medication may be prescribed.
Common medications for narcolepsy include modafinil, IR-MPH, and OROS-MPH. These medications have been proven to dramatically increase the quality of life for those with narcolepsy. As there is no known cure, scientists are avidly working on ways to improve narcolepsy symptoms. Recently, a study was published stating that “once-nightly sodium oxybate, called FT218, was shown to significantly improve symptoms of narcolepsy compared with placebo while also maintaining a safety profile similar to that of sodium oxybate”. This article, published in August of 2021, said that 72% of those given this medication had a better score by 95% on their illness severity test. Because of this, they are seeking approval from the FDA to roll out this new type of medication.
Another article published in June of 2021 suggests that immunotherapy may benefit those with narcolepsy. This article suggests that narcolepsy might be a new autoimmune disease and, therefore, can be treated with immunotherapy like other autoimmune diseases. The data within the article is mixed and, therefore, requires further testing. However, those with type 1 narcolepsy, the type with cataplexy, had dramatic changes in their symptoms. According to this article, they will be conducting a double-blind, randomized, placebo-controlled trial sometime in the near future.
According to this final article, published in August of 2o21, race may play a factor in determining what type of narcolepsy a patient has. This study found that those with Hispanic and Latino backgrounds may be more apt to have early onset narcolepsy which starts affecting children at the age of 10. This is important because if scientists can find the gene responsible for narcolepsy, they may be able to target that gene specifically in treatment, betting the chances of finding a cure. This article states that more studies will need to be conducted in the future to determine if there is a true correlation between race and narcolepsy.
Refrences:
“The Science of Narcolepsy”; healthysleep.med.harvard.edu; https://healthysleep.med.harvard.edu/narcolepsy/what-is-narcolepsy/science-of-narcolepsy
“High Prevalence of Eating Disorders in Narcolepsy with Cataplexy: A Case-Control Study”; ncbi.nlm.nih.gov; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2276738/
“Cataplexy”; sleepfoundation.org; https://www.sleepfoundation.org/physical-health/cataplexy
“Depression occurs often in narcolepsy, but improves with treatment of sleep disorder”; www.healio.com; https://www.healio.com/news/neurology/20201001/depression-occurs-often-in-narcolepsy-but-improves-with-treatment-of-sleep-disorder
“Experience with the use of modafinil in the treatment of narcolepsy in a outpatient facility specialized in diurnal excessive sleepiness in São Paulo”; ncbi.nlm.nih.gov; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4521685/
“The Economic Consequences of Narcolepsy”; ncbi.nlm.nih.gov; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2699169/